How to heal a fistula without surgery, is a most important question because everyone thinks that fistula cannot be cured without surgery but this is not true.
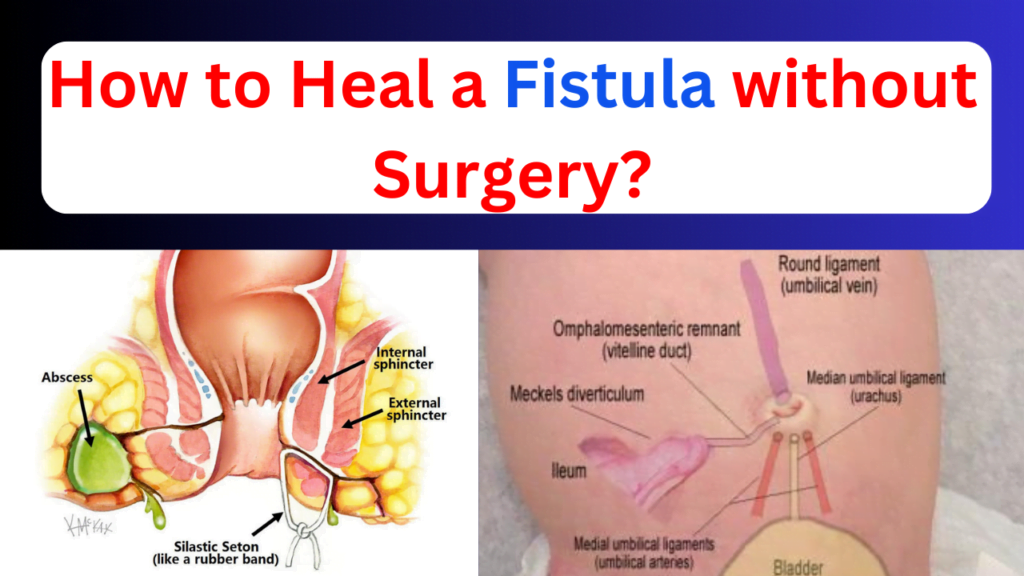
A fistula, an abnormal connection between two structures or body areas, can arise from various causes, including injury, surgery, infection, or inflammation. These abnormal connections may manifest in different parts of the body, such as between the throat and neck, the colon and nearby skin, or an artery and vein.
One specific type is the anal fistula, characterized by an infected tunnel between the anus and perianal skin, with its exterior entrance located at the anal opening. To manage this condition, individuals are advised to increase fluid intake, particularly water, and maintain a balanced, high-fiber diet. This dietary approach aims to promote the development of soft stools, reducing the pressure required for bowel movements. This is especially beneficial for those with anal fistulas, as passing firm stools can be both unpleasant and challenging. Additionally, maintaining proper hygiene when using the restroom is crucial to prevent infections and mitigate other associated complications.
Anal Fistula
Table of Contents
Understanding Anal Fistulas: Unraveling the Connection Between Anus and Perianal Skin
An anal fistula refers to an infected tunnel that forms between the anus and the perianal skin, with one end situated at the anal opening. Typically, individuals who previously experienced an anal abscess are prone to discovering the presence of a fistula. However, other underlying severe conditions, such as Crohn’s disease, cancer, warts, radiation, or trauma, can also contribute to the development of a fistula.
Notably, a sedentary lifestyle and lack of regular physical activity, particularly in obese individuals, are often associated with complaints of fistulas. Adults, as opposed to children, are more susceptible to experiencing this condition. Moreover, individuals with perianal abscesses face a significant risk of developing an anal fistula. This article delves into the intricacies of anal fistulas, exploring their origins, associated risk factors, and potential connections to various health conditions.
Symptoms of Anal Fistulas: Recognizing the Signs
Anal fistulas manifest through various symptoms, offering crucial insights into their presence. Understanding these indicators can aid in early detection and prompt medical intervention. Here are the key symptoms associated with anal fistulas:
- Anal Discomfort:
- The anal opening becomes a focal point for symptoms, presenting with pain, swelling, itching, irritation, or sore skin. These discomforting sensations often signal the presence of an anal fistula.
- Bleeding:
- A notable symptom includes the discharge of blood. Individuals with anal fistulas may observe blood during bowel movements, indicating a potential issue in the anal region.
- Painful Bowel Movements:
- Bowel movements can become a source of pain for individuals with anal fistulas. The discomfort may intensify as the illness progresses, making routine activities such as bowel movements increasingly challenging.
- Pain during Urination:
- In advanced stages, patients may experience pain while urinating. This additional symptom underscores the impact of anal fistulas on nearby structures and functions.
- Systemic Symptoms:
- Fever and exhaustion are systemic symptoms that may accompany anal fistulas. These indicators suggest that the body is responding to the infection, and medical attention is warranted.
- Foul Odor:
- Another distinctive symptom is the presence of discharge with a foul odor emanating from the anal aperture. This olfactory element can be indicative of the infectious nature of the fistula.
How to heal a fistula without surgery
A brief overview of fistulas and their typical treatment methods
A fistula is an abnormal connection or passageway between two organs, vessels, or structures that are not naturally connected. Fistulas can occur in various body parts, such as the gastrointestinal tract, urinary system, or skin. They often result from infections, inflammation, trauma, or complications of certain medical conditions.
Typical Treatment Methods for Fistulas
1. Surgical Intervention:
a- Abscess Drainage: If a fistula is associated with an abscess, surgical drainage is often performed to remove the pus and alleviate symptoms.
b- Fistulotomy: A common surgical procedure where the fistula tract is opened and the contents are drained, promoting healing.
c- Seton Placement: Involves placing a seton (a thread or rubber band) through the fistula to facilitate drainage and prevent closure.
2. Medication:
a- Antibiotics: Prescribed to treat or prevent infections associated with fistulas.
b- Immunosuppressive Drugs: In cases where fistulas are linked to autoimmune conditions like Crohn’s disease, medications to modulate the immune response may be recommended.
3. Non-Surgical Approaches:
a- Dietary Changes: High-fiber diets may be suggested to promote softer stools, reducing strain during bowel movements.
b- Hygiene Practices: Maintaining cleanliness in the affected area to prevent infection and promote healing.
c- Sitz Baths: Warm water baths that can help alleviate pain and discomfort associated with certain types of fistulas.
4. Treating Underlying Conditions:
Identifying and addressing the underlying causes of fistula formation, such as inflammatory bowel disease, cancer, or infections.
5. Regular Monitoring:
Periodic monitoring of symptoms and follow-up appointments with healthcare providers to track progress and adjust treatment plans as needed.
Individuals with fistulas need to consult with healthcare professionals for accurate diagnosis and personalized treatment plans. The choice of treatment depends on factors like the type and location of the fistula, underlying health conditions, and the severity of symptoms. Early intervention and appropriate medical guidance are key to effective management and optimal outcomes to know how to heal a fistula without surgery.
Section 1: Introduction (How to heal a fistula without surgery)
In the realm of medical interventions, the concept of non-surgical approaches for healing fistulas has emerged as a promising avenue, offering individuals alternative methods to address these abnormal connections. While surgical interventions remain prevalent, the recognition of non-surgical strategies reflects a growing awareness of holistic and less invasive options for how to heal a fistula without surgery.
Overview of Fistula Types: Exploring how to heal a fistula without surgery.
Fistulas, abnormal connections between bodily structures, come in various forms, each presenting unique challenges and considerations. Understanding the diversity of fistula types is crucial in tailoring effective approaches to their management. While surgical interventions have traditionally been the go-to solution, there is a growing acknowledgment that non-surgical methods can be viable alternatives for addressing specific types of fistulas.
Different Types of Fistulas:
1. Anal Fistulas:
Formed between the anus and perianal skin, often associated with infections. Non-surgical approaches may play a role in managing symptoms and promoting healing.
2. Vesicovaginal Fistulas:
Connecting the bladder to the vagina, typically resulting from childbirth complications. Non-surgical options may complement conventional treatments in certain cases.
3. Enterocutaneous Fistulas:
Involving abnormal connections between the intestine and the skin. Dietary adjustments and medical management can be considered for non-surgical support.
4. Arteriovenous Fistulas:
Formed between arteries and veins, either congenital or acquired. While surgical correction is common, non-surgical monitoring may be appropriate in certain situations.
5. Gastrocolic Fistulas:
Connecting the stomach and colon, often associated with conditions like cancer. Dietary modifications and symptom management are essential components of non-surgical care.
Understanding that not all fistulas require immediate surgical intervention, this overview aims to emphasize the potential role of non-surgical approaches in the comprehensive management of diverse fistula types. From lifestyle adjustments to medical therapies, exploring alternative methods can contribute to a more nuanced and personalized approach to addressing the complex nature of fistulas.
Section 2: Common Causes of Fistulas
The development of fistulas is often rooted in a variety of common factors that contribute to their formation. Understanding these underlying causes is pivotal in devising effective strategies for prevention and management. This exploration sheds light on prevalent factors leading to the emergence of fistulas, encompassing infections, abscesses, and underlying health conditions.
1. Infections:
Infection is a primary catalyst for fistula development. When infections occur in specific bodily structures or organs, they can lead to the formation of abscesses, subsequently evolving into fistulas. Common sources include bacterial or viral agents that initiate inflammation and tissue damage.
2. Abscess Formation:
The presence of abscesses, and localized collections of pus, is a significant precursor to fistula development. Abscesses can arise from infections, trauma, or complications of pre-existing medical conditions. When these abscesses fail to resolve, they may create abnormal passageways, giving rise to fistulas.
3. Underlying Health Conditions:
Various underlying health conditions can predispose individuals to fistula development. Inflammatory bowel diseases, such as Crohn’s disease, are notorious for their association with fistulas. Additionally, conditions like cancer, radiation therapy, or chronic illnesses can contribute to the weakening of tissues and the subsequent formation of abnormal connections.
By delving into these common factors, we gain a comprehensive understanding of the intricate processes leading to fistula genesis. Recognizing the role of infections, abscesses, and underlying health conditions is pivotal not only for early detection, but also for developing targeted interventions aimed at addressing these root causes and preventing the progress on how to heal a fistula without surgery.
The intricate relationship between lifestyle choices and the development or exacerbation of fistulas underscores the importance of holistic well-being in preventing and managing these abnormal connections. While medical factors play a significant role, certain lifestyle choices can contribute to the predisposition or worsening of fistulas.
1. Sedentary Habits:
Prolonged periods of sitting, common in sedentary lifestyles, can lead to increased pressure on the pelvic region. This pressure, coupled with reduced blood flow, may contribute to the development or exacerbation of fistulas, particularly in the anal and rectal areas.
2. Poor Dietary Habits:
Diets lacking in fiber can result in constipation and hard stools, increasing the strain during bowel movements. This heightened pressure may contribute to the formation of anal fistulas and worsen symptoms associated with existing fistulas.
3. Hygiene Practices:
Inadequate hygiene practices, such as improper cleansing after bowel movements, may lead to recurrent infections in the perianal region. These infections, if left untreated, can contribute to the development of fistulas.
4. Obesity:
Being overweight or obese is often associated with an increased risk of developing fistulas. Excess weight can exert pressure on various bodily structures, potentially contributing to the formation of abnormal connections.
5. Smoking:
Smoking has been linked to delayed wound healing and compromised immune function. In the context of fistulas, these effects may impede the natural healing process, making individuals more susceptible to persistent or recurrent fistula-related issues.
Understanding the impact of lifestyle choices on fistula development allows individuals to adopt preventive measures. Incorporating regular physical activity, maintaining a high-fiber diet, practicing proper hygiene, achieving, and maintaining a healthy weight, and abstaining from smoking are pivotal steps in promoting overall health and potentially mitigating the risk or severity of fistulas. This holistic approach complements medical interventions and fosters a comprehensive strategy for managing and preventing these abnormal connections.
Reasons For Fistula–https://youtu.be/pQYglVCUDsI
Section 3: Non-Surgical Healing Approaches
1. Nourishment for Healing: The Impact of a High-Fiber Diet on Fistula Management
A cornerstone in the holistic management of fistulas lies in the transformative power of a healthy, high-fiber diet. This dietary approach not only plays a pivotal role in promoting natural healing but also serves as an effective strategy for alleviating symptoms associated with fistulas. How to heal a fistula without surgery is a crucial question and one of the best answers is a high-fiber diet.
1. Softening Stools and Reducing Strain:
A high-fiber diet, rich in fruits, vegetables, and whole grains, contributes to the formation of soft and bulky stools. This softening effect minimizes the strain during bowel movements, a crucial factor in easing discomfort associated with fistulas, particularly in the anal and rectal regions.
2. Enhanced Digestive Health:
Fiber is renowned for its digestive benefits, promoting regular bowel movements and preventing constipation. By maintaining optimal bowel function, a high-fiber diet helps prevent the recurrence of abscesses and minimizes the risk of new fistula formations.
3. Nutrient Absorption and Immune Support:
Whole, nutrient-dense foods integral to a high-fiber diet support overall health and aid in the absorption of essential nutrients. Adequate nutrition fortifies the body’s immune system, enhancing its capacity to combat infections and contributing to the natural healing process.
4. Inflammation Management:
Fiber possesses anti-inflammatory properties, which can be particularly beneficial for individuals with fistulas associated with inflammatory conditions such as Crohn’s disease. Managing inflammation is instrumental in reducing symptoms and fostering an environment conducive to healing.
5. Balancing Gut Microbiota:
A high-fiber diet promotes a healthy balance of gut microbiota. This microbial equilibrium is crucial for maintaining gastrointestinal health and may play a role in preventing complications related to fistulas.
Incorporating a high-fiber diet into the daily routine emerges as a proactive and empowering step in fistula management. Not only does it address symptoms directly linked to bowel movements, but it also contributes to the overall well-being of individuals navigating the challenges of fistula-related concerns. Coupled with other lifestyle modifications and medical interventions, a nutrient-rich, high-fiber diet emerges as a valuable ally in the journey towards natural healing and improved quality of life.
2. Prioritizing Hygiene: A Crucial Element in Preventing Infection and Fostering how to heal a fistula without surgery.
Maintaining proper hygiene is an indispensable aspect of managing fistulas, playing a pivotal role in preventing infections and expediting the healing process. The significance of stringent hygiene practices cannot be overstated, as they directly impact the overall well-being of individuals contending with fistula-related challenges.
1. Infection Prevention:
Proper hygiene practices act as a formidable line of defense against infections, a common complication associated with fistulas. Regular cleansing of the affected area helps mitigate the risk of bacterial infiltration, reducing the likelihood of recurrent infections that can impede the healing process.
2. Promoting Healing:
Cleanliness is closely linked to the facilitation of the natural healing process. By keeping the affected area free from contaminants, individuals create an environment conducive to tissue repair and regeneration. This, in turn, contributes to a more expedited and effective healing trajectory.
3. Reducing Discomfort:
Pristine hygiene not only prevents infections but also alleviates discomfort. Irritation and itching, common symptoms of fistulas, can be mitigated through diligent cleansing, promoting a more comfortable and manageable experience for individuals navigating this health concern.
4. Preventing Complications:
Complications arising from poor hygiene, such as worsening of symptoms or the development of additional infections, can be avoided through consistent and thorough cleanliness practices. Proactive hygiene measures act as a safeguard against potential setbacks in the recovery journey.
5. Enhancing Overall Well-Being:
Beyond the immediate effects on fistula management, maintaining proper hygiene contributes to the overall physical and emotional well-being of individuals. Feeling clean and hygienic fosters a sense of confidence and control, positively impacting the quality of life during the healing process and to know how to heal a fistula without surgery.
In essence, proper hygiene emerges as an empowering and preventative measure in the comprehensive care of fistulas. By embracing meticulous cleanliness practices, individuals not only shield themselves from potential complications but also actively support the body’s innate capacity for healing. As an integral component of a holistic approach, prioritizing hygiene stands as a proactive and effective strategy in the journey toward optimal fistula management and improved health outcomes.
3. Sitz Baths and Warm Compresses
Embracing Comfort: The Therapeutic Benefits of Warm Water Treatments for Fistula Relief and Healing
In the realm of fistula management how to heal a fistula without surgery, the therapeutic influence of warm water treatments stands as a noteworthy ally, offering relief from pain and contributing to the overall healing process. This exploration unveils the multifaceted benefits of incorporating warm water into the care regimen, showcasing its potential to alleviate discomfort and promote the restoration of well-being.
1. Pain Relief:
Warm water serves as an effective cleansing agent, aiding in the removal of discharge and debris and how to heal a fistula without surgery. This cleansing action, not only supports hygiene practices, but also contributes to the prevention of secondary infections that may impede the healing process.
2. Muscle Relaxation:
The warmth of the water induces muscle relaxation, especially beneficial for those with anal or rectal fistulas. Relaxed muscles minimize tension in the affected area, contributing to a tangible reduction in pain and enhancing the overall sense of comfort.
3. Improved Blood Circulation:
Warm water treatments enhance blood circulation to the affected region. Improved blood flow facilitates the delivery of oxygen and nutrients to the injured tissues, fostering an environment conducive to natural healing and cellular regeneration.
4. Cleansing and Hygiene:
Warm water serves as an effective cleansing agent, aiding in the removal of discharge and debris that how to heal a fistula without surgery. This cleansing action, not only supports hygiene practices, but also contributes to the prevention of secondary infections that may impede the healing process.
5. Stress Reduction:
Beyond the physical benefits, warm water treatments offer a psychological respite. Immersion in warm water induces a sense of relaxation, helping individuals manage the emotional toll often associated with fistula-related challenges.
6. Promoting Healing Environment:
The gentle nature of warm water treatments creates an environment conducive to healing. By promoting a state of relaxation and comfort, warm water contributes to the body’s ability to naturally repair and restore tissues affected by the fistula.
Incorporating warm water fistula treatments into the overall care strategy for fistulas emerges as a holistic and comforting approach. Beyond pain relief, the benefits extend to improved hygiene, stress reduction, and the creation of an environment that actively supports the body’s innate healing mechanisms. As a complementary measure, the therapeutic embrace of warm water enriches the journey toward alleviating discomfort and fostering optimal healing for individuals navigating the complexities of fistula treatment.
4. Herbal Remedies and Supplements
Harnessing Nature’s Remedies: Herbs and Supplements for how to heal a fistula without surgery.
In the pursuit of how to heal a fistula without surgery, the realm of herbal remedies and supplements offers a promising avenue, showcasing specific natural elements renowned for their potential to support the healing process. This discussion delves into noteworthy herbs and supplements recognized for their therapeutic properties, aiming to shed light on their role in promoting optimal recovery from fistula treatment-related challenges.
1. Turmeric:
Active Ingredient: Curcumin
Benefits: Renowned for its anti-inflammatory properties, turmeric may aid in reducing inflammation associated with fistulas. Its antioxidant effects also contribute to tissue repair.
2. Aloe Vera:
Active Ingredients: Polysaccharides, glycoproteins
Benefits: Aloe vera’s soothing and anti-inflammatory properties can provide relief from discomfort. Its application may support the healing of external fistula openings.
3. Calendula:
Active Ingredients: Flavonoids, triterpenoids
Benefits: Calendula’s anti-inflammatory and antimicrobial properties make it a potential ally in wound healing, aiding in the management of fistula-related symptoms.
4. Chamomile:
Active Ingredients: Apigenin, bisabolol
Benefits: Chamomile’s anti-inflammatory and calming effects may help alleviate pain and discomfort associated with fistulas. It is often used topically or in warm compresses.
5. Bromelain:
Derived from Pineapple
– Benefits: Bromelain, known for its anti-inflammatory and anti-swelling properties, may contribute to reducing inflammation and supporting the natural healing process.
6. Vitamin C:
Benefits: As a powerful antioxidant, vitamin C plays a crucial role in collagen synthesis and immune function. Adequate vitamin C intake is essential for tissue repair and overall immune support.
7. Zinc:
Benefits: Zinc is vital for wound healing and immune function. It supports the body’s ability to repair tissues, making it a valuable supplement for individuals managing fistulas.
8. Probiotics
Benefits:
Probiotics contribute to gut health and may be beneficial for individuals with fistulas related to gastrointestinal conditions. Maintaining a healthy gut microbiota can support overall well-being and promote how to heal a fistula without surgery.
While these herbs and supplements show promise, it is crucial to consult healthcare professionals before incorporating them into one’s regimen. Individual responses vary, and expert guidance ensures safe and effective integration into a personalized approach to fistula healing. The synergy of natural remedies, lifestyle modifications, and conventional medical interventions can contribute to a comprehensive strategy in navigating the complexities of fistula treatment.
5. Homeopathy: How to heal a fistula without surgery
Homeopathic medicine is a system of alternative medicine that relies on the principles of “like cures like” and the use of highly diluted substances to stimulate the body’s natural healing processes. While some individuals may choose to explore homeopathic remedies for various health conditions, it’s important to note that the efficacy of such fistula treatments can vary, and individual responses may differ. Here are some homeopathic medicines that have been historically considered in the context of how to heal a fistula without surgery:
1. Silicea:
Indications: Silicea is often suggested when there is a tendency for recurrent abscesses and slow-healing wounds. It may be considered for promoting suppuration and drainage in certain cases and it acts a best medicine for fistula treatment to know, how to heal a fistula without surgery.
2. Myristica Sebifera:
Indications: Myristica sebifera is associated with aiding the natural drainage of pus and supporting the healing of abscesses. It is sometimes considered in cases of anal fistulas.
3. Calcarea Sulphurica:
Indications: This remedy is often associated with promoting the healing of wounds and may be considered when there is a discharge of yellow pus from the fistula.
4. Hepar Sulph:
Indications: Hepar sulph is suggested when there is sensitivity to touch, and the fistula is associated with the formation of abscesses or when there is offensive-smelling discharge.
5. Thuja Occidentalis:
Indications: Thuja is often considered when there is a history of vaccination or suppression of skin conditions. It may be chosen based on individual symptoms and constitutional factors.
6. Sulphur:
Indications: Sulphur is associated with promoting general detoxification and supporting skin health. It may be considered in certain cases of chronic or recurrent anal fistulas.
It is crucial to emphasize that the selection of homeopathic remedies should be individualized, considering the specific symptoms, overall health, and constitutional factors of the individual. Homeopathic treatment is best undertaken under the guidance of a qualified homeopathic practitioner who can tailor the remedies to the unique characteristics of the person seeking treatment.
It’s important to note that while some people may find relief from homeopathic treatments, others may prefer conventional medical approaches, such as fistula surgery or medication, for managing anal fistulas. For an accurate diagnosis and appropriate treatment plan, always consult a healthcare professional.
Section 4: When to Seek Professional Advice
(a) Monitoring Symptoms
Knowing When to Seek Medical Attention for Fistula Symptoms: A Guide
While certain strategies can be employed at home for comfort, it is crucial to recognize when the fistula symptoms associated with a fistula warrant immediate medical attention. Timely intervention is essential to prevent complications and ensure effective management. Consider seeking medical attention under the following circumstances:
1. Persistent Pain:
If the pain associated with the fistula is severe, persistent, or worsening despite home care measures, it is advisable to consult a healthcare professional. Uncontrolled pain may indicate underlying issues requiring medical assessment and intervention.
2. Increased Discharge or Foul Odor:
An increase in the amount of discharge from the fistula or the presence of a foul odor may indicate infection or complications. If there is a noticeable change in the characteristics of the discharge, seeking medical attention is advisable.
3. Fever and Chills:
The development of fever and chills suggests an inflammatory response or infection. Elevated body temperature may indicate a systemic issue that requires medical evaluation to determine the appropriate course of action.
4. Worsening Symptoms:
If the overall symptoms, such as swelling, redness, or discomfort, are intensifying over time, it is essential to consult with a healthcare provider. Worsening symptoms may signify an evolving condition that necessitates professional evaluation.
5. Difficulty with Bowel Movements:
If there are difficulties with bowel movements, such as persistent constipation or increased pain during defecation, medical attention is warranted. These issues may be indicative of complications that require assessment and intervention.
6. Development of New Symptoms:
The emergence of new symptoms, unrelated to typical fistula characteristics, should be promptly addressed. Any unusual or concerning changes in health should be discussed with a healthcare professional for a comprehensive evaluation.
7. Previous Treatments Yield No Improvement:
If home care measures or previous treatments have provided little to no improvement in symptoms, it is crucial to consult with a healthcare provider. Persistent or recurring issues may require a reassessment of the treatment plan.
Remember that every individual’s situation is unique, and the severity of symptoms can vary. If you have concerns about your health, trust your instincts and seek medical attention. Early intervention can lead to more effective management and improved outcomes in the treatment of fistulas.
(b) Consulting Healthcare Professionals
Prioritizing Professional Guidance: The Crucial Role of Healthcare Professionals in Fistula Care
Navigating the complexities of fistula management necessitates the expertise and guidance of healthcare professionals. While home care measures can offer relief, they are not substitutes for a comprehensive assessment and tailored treatment plan. Emphasizing the importance of consulting healthcare professionals is fundamental to ensuring accurate diagnosis and effective guidance throughout the healing journey.
1. Accurate Diagnosis:
Healthcare professionals possess the knowledge and tools needed to conduct thorough assessments and provide accurate diagnoses. A precise understanding of the type, location, and severity of the fistula is paramount in developing an appropriate treatment strategy.
2. Tailored Treatment Plans:
Fistulas vary widely, and their management requires individualized approaches. Healthcare professionals can formulate tailored treatment plans that address specific symptoms, underlying causes, and the overall health of the individual. This personalized care enhances the likelihood of successful outcomes.
3. Identification of Underlying Conditions:
Fistulas can be associated with underlying health conditions such as inflammatory bowel disease or infections. Healthcare professionals are equipped to identify and address these contributing factors, offering a comprehensive approach to healing.
4. Monitoring Progress:
Regular follow-ups with healthcare professionals allow for the monitoring of progress and the adjustment of treatment plans as needed. This ongoing collaboration ensures that interventions remain effective and aligned with the individual’s evolving health status.
5. Prescription of Medications:
In certain cases, medications such as antibiotics or anti-inflammatory drugs may be prescribed to manage infections or alleviate symptoms. Healthcare professionals can determine the appropriate medications and dosages based on the specific needs of the individual.
6. Guidance on Lifestyle Modifications:
Healthcare professionals can provide valuable guidance on lifestyle modifications that complement medical interventions. This may include dietary changes, physical activity recommendations, and hygiene practices that promote overall well-being.
7. Addressing Emotional and Psychological Aspects:
Living with a fistula can have emotional and psychological implications. Healthcare professionals, including mental health specialists, can offer support, address concerns, and provide coping strategies to enhance the individual’s overall quality of life.
In essence, consulting healthcare professionals is not just a step in the journey of managing fistulas; it is a cornerstone. Their expertise ensures that individuals receive comprehensive care, from accurate diagnosis to ongoing support. Seeking professional guidance empowers individuals to make informed decisions about their health, fostering a collaborative and proactive approach to fistula care.
Conclusion
Non-surgical approaches for fistula management offer a multifaceted toolkit for individuals seeking alternatives to surgical interventions. These strategies, when applied thoughtfully and under professional guidance, contribute to a comprehensive and personalized approach to promoting healing, managing fistula symptoms, and fostering overall well-being in the context of fistulas.
Empowering the Journey: Exploring Non-Surgical Approaches with Professional Guidance
Embarking on the path of non-surgical approaches for managing fistulas is a proactive and empowering choice. As you consider incorporating dietary changes, hygiene practices, warm water treatments, herbal remedies, and lifestyle modifications into your routine, it’s essential to do so under the watchful guidance of healthcare professionals. Here’s a word of encouragement:
Your Health, Your Journey:
Your well-being is a unique and precious journey, and exploring non-surgical methods aligns with a holistic approach to fistula management. Each step you take toward healing is a testament to your commitment to a healthier, more comfortable life.
The Expertise of Healthcare Professionals:
While these non-surgical strategies offer promise, it’s crucial to undertake this journey under the guidance of healthcare professionals. Their expertise ensures that your approach is tailored to your specific symptoms, type of fistula, and overall health. Seeking professional supervision is a proactive step toward optimal outcomes.
A Collaborative Effort:
Healthcare professionals are your allies in this endeavor, providing not just medical expertise but also a supportive partnership. They can offer insights, monitor progress, and adjust your plan as needed. Together, you form a collaborative team dedicated to your well-being.
Precision in Personalization:
The beauty of non-surgical approaches lies in their potential for personalization. What works for one person may not work for another. With the guidance of healthcare professionals, you can navigate this realm with precision, ensuring that the chosen strategies align seamlessly with your unique health profile.
Celebrating Progress, Embracing Wellness:
As you embrace non-surgical methods, celebrate every small victory, and acknowledge the progress you make. Each positive step contributes to your overall wellness. Remember, it’s not just about managing the symptoms; it’s about cultivating a lifestyle that supports your well-being.
You Are Not Alone:
In this journey, you are not alone. Healthcare professionals are there to listen, understand, and support you. Seek their guidance, share your concerns, and together, you can build a roadmap to better health.
In Closing:
Exploring non-surgical approaches are a commendable choice—one that reflects your commitment to a balanced and holistic approach to healing. With the guidance of healthcare professionals, your journey becomes not just a path to fistula symptom relief but a transformative exploration of well-being. Here’s to your health, your empowerment, and the promising road ahead.